Both the kidneys together receive 1.2 lit/ minute as blood flow, which are about 25% of cardiac output. The cortex receives 90% of blood flow, while the medulla receives only 10%. The inner medulla receives only 1 to 2% of the renal blood flow. The sluggish blood flow of the inner medulla helps in maintaining the high osmolality of that region.
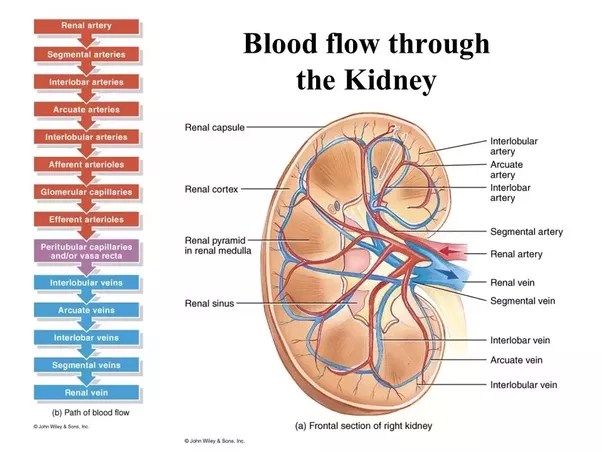
The renal circulation begins with the renal artery breaking into interlobar arteries. These in turn open into arcuate arteries, which run along the base of the papillae of the kidney. From arcuate artery, interlobular arteries arise and go to cortex of the kidney. From interlobular artery, afferent arteriole is given off and from which arises glomerular capillary tuft. They unite and form the efferent arteriole. It continues as the vasa recta in the case of juxtamedullary nephrons and peritubular capillary in the cortical nephrons. The vasa recta supplies the loop of Henle, DCT, collecting duct and the neighbouring nephrons.
The venous drainage begins with the vasa recta opening into the interlobular vein and then into the arcuate vein. This in turn drains into the interlobar vein, which finally opens into the renal vein. The renal blood flow can be measured by the Fick’s principle. The substance used to measure is PAH (para-aminohippuric acid) or Diodrast. These substances are secreted from the peritubular capillaries into the lumen of the PCT. In one circulation, about 90% is secreted from the renal blood flow.
Renal PAH clearance measure renal plasma flow. In the determination of PAH clearance, the arterial plasma concentration of PAH is considered. Since the renal venous blood PAH concentration is not measured, the PAH clearance gives only the effective renal plasma flow ( ERPF). The unique feature of the renal blood flow is its autoregulation. The RPF and GFR remain constant inspite of variations in the mean arterial blood pressure from 90 to 200 mmHg.
There are two mechanisms, which can explain the autoregulation. The reflex constriction of afferent arteriole, when renal perfusion pressure is increased, leads to restoration of normal RBF and GFR. The mechanism is independent of extrinsic nerve supply of the afferent arteriole and is due to the property of the smooth muscle lining the afferent arteriole. It refers to the feedback from the renal tubules, which helps to maintain GFR. Whenever the rate of flow is decreased in the tubule, due to fall in GFR, the sodium reaching the first part of the distal tubule called macula densa will be reduced. This is sensed by the macula densa cells, which in turn causes dilatation of the afferent arteriole and at the same time, the release of renin from juxta glomerular cells, leads to the formation of angiotensin II. This causes constriction of the efferent arteriole. The net effect is increase of glomerular hydrostatic pressure and GFR. Conversely, when the rate of flow is increased due to rise in GFR, the GFR is reduced by the vasoconstriction of the afferent arteriole. The arteriolar constriction may also be due to the release of thromboxane A2.
Renal blood flow to the renal cortex is high but oxygen consumption is low whereas the blood flow to the medulla is low but the oxygen utilisation is high as the ascending loop of Henle is involved in active Na+ reabsorption. Renal blood vessels are supplied by the sympathetic nerves and its stimulation causes reduction in renal blood flow and GFR. The sympathetic stimulation to the kidneys also causes release of renin.
Source: Textbook of Physiology, 3E (Chandramouli) (2010)