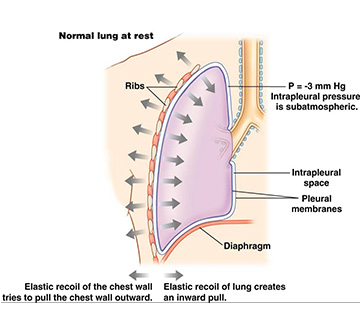
During respiration, there are pressure and volume changes in the alveoli. The lungs are lined by the visceral pleura, whereas, the thoracic wall is lined by the parietal pleura. The space between these two is the intrapleural space. There is a thin serous fluid present in the space, which gives hydraulic traction between these two layers. This makes them inseparable. The pressure between these two layers is called intrapleural pressure. The intrapleural pressure is subatmospheric.
The first breath, which occurs at the time of birth, establishes a negative pressure in the intrapleural space. The lungs, because of its elastic structure, try to recoil, while the chest wall tends to pull outwards at the end of quiet expiration, creating a negative pressure in the intrapleural space. The intrapleural pressure is – 2.5 mmHg at the beginning of inspiration and becomes – 6 mmHg at the end of inspiration. During expiration, it becomes less negative and reaches the preinspiratory level. Forceful inspiration causes intrapleural pressure to become more negative, reaching up to – 30 mmHg. The negative intrapleural pressure prevents the collapse of alveoli during expiration. Further, it makes the alveoli distended during inspiration. This is the major function of intrapleural pressure, which gives stability to the lungs. Pneumothorax refers to the entry of air into the intrapleural space. The lung collapses in such a condition.
The intrapleural pressure can be measured by introducing into the mouth, a catheter with an inflatable balloon at the tip and positioned in the mid esophageal region. The other free end is connected to a pressure transducer for recording the pressure changes. Since the esophageal pressure reflects the intrapleural pressure, this method is considered accurate.
In standing posture, the effect of gravity on intrapleural pressure can be seen. There is a gradient from the basal part of lungs to the apex, with the apex showing more negative pressure (– 10 mmHg) and the basal part having less negative pressure (– 2 mmHg). That’s why, the apical portion has more resting volume of air, but less ventilated, as compared to the basal part of lungs.
Source: Textbook of Physiology, 3E (Chandramouli) (2010)