B-Cell Development
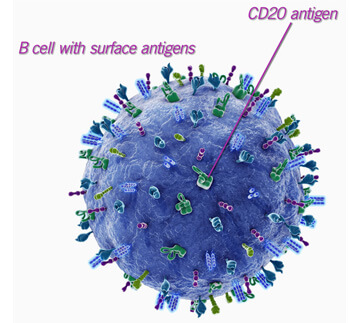
B cells constitute approximately 10% of peripheral blood leukocytes. They develop in the bone marrow from hematopoietic stem cells but achieve maturity in peripheral lymphoid organs. Early progenitors committed to the B-cell lineage (pro–B cells) begin recombination at the immunoglobulin heavy-chain loci. Successful recombination leads to expression of μ–heavy chain, distinguishing them from pre–B cells. With the surrogate light chain and the Ig-α/β signaling machinery, an immunoglobulin-like heterodimer is expressed on the surface (pre–B-cell receptor). The pre–B-cell receptor signals a halt to μ–heavy-chain recombination, and Igκ or Igλ light-chain recombination begins. The surrogate light chain is replaced by a successfully formed κ or λ light chain, and the B-cell receptor is expressed as surface IgM, which distinguishes the immature B cell.
B-Cell Responses
B cells provide humoral immunity against extracellular pathogens through the production of antibodies that neutralize pathogens and toxins, facilitate opsonization, and activate complement. Primary infection or vaccination results in prolonged production of high-affinity specific antibodies, the basis of adaptive humoral immunity. On the other hand, IgM antibodies are produced in the absence of infection, are of lower affinity, play a role in first-line defense against bacterial infection, and assist in clearance of endogenous cellular debris. Naïve follicular B cells reside in the follicles of secondary lymphoid tissues. Antigen arrives in these lymphoid organs through circulation of soluble molecules or immune complexes or via transportation by dendritic cells. The B cells, via the B-cell receptors, process the antigens in the context of MHC class II and then migrate to the T cell–B cell interface, the border between the T-cell zone and B-cell follicle, where they encounter primed TH cells of cognate specificity. This generates signals from T-cell–derived cytokines and triggers binding between CD40 ligand (CD40L, on T cells) and CD40 (on B cells) that sustains B-cell activation and promotes immunoglobulin class switching. Signaling through CD40 and its interaction with CD40 ligand on T cells is essential for the induction of isotype switching.
The effector T-cell cytokines have various functions: IL-1 and IL-2 promote B-cell activation and growth, IL-10 causes switching to IgG1 and IgG3, IL-4 and IL-13 cause switching to IgE, and TGF-β causes switching to IgA. IFN-γ, or some other undefined product of TH1 cells, appears to induce switching to IgG2. Activated B cells either migrate into the follicle and, with continued T-cell help, initiate the germinal center reaction or migrate to the marginal zone and differentiate into short-lived plasma cells. These latter cells secrete antibody for 2 to 3 weeks, which provides a rapid but transient source of effector molecules.
The B cells in the germinal center undergo specificity diversification through somatic hypermutation, and high-affinity variants are selected by survival advantage, a process termed affinity maturation. Thus within the germinal centers, sequential cycles of proliferation, B-cell receptor diversification, and selection amplify high-affinity variants of the original activated B cell. The cells that then exit the germinal center reaction give rise to the memory compartment, which consists of affinity-matured memory B cells and long-lived plasma cells. When memory cells reencounter antigen, they divide rapidly and expand their numbers or differentiate into antibody-secreting plasma cells. These long-lived plasma cells are terminally differentiated B cells incapable of further division that home to the bone marrow and secrete high-affinity class-switched antibody. These B cell responses are orchestrated with the help of T cells and their cytokines and are termed T-cell–dependent B-cell responses.
Source: Cummings Otolaryngology, 6E (2015)